Introduction: Hematopoietic stem cell transplantation (HSCT) improves long term overall survival (OS) and disease-free survival (DFS) in those with intermediate or high-risk B- cell ALL. Historically, matched related donors were the ideal choice, but with improved GVHD prophylactic regimens and supportive care, haploidentical donors are being increasingly used. Due to their increased graft-versus-leukemia (GVL) effect, they may be an option for Hispanic patients, for whom matched donation may be more challenging.
Methods: This is a retrospective chart review of B- cell ALL patients that received allogeneic HSCT at Norris Comprehensive Cancer Center (NCCC) from 2012 to 2023. Mismatch-unrelated donors were excluded. For OS, DFS, and cumulative incidence of relapse (CIR), match sibling donors (MSD) and match unrelated donors (MUD) were grouped. However, for GVHD outcomes including graft-versus-host disease (GVHD)-free relapse-free survival (GRFS), incidence of grade 3-4 acute GVHD (aGVHD), and incidence of severe chronic GVHD (cGVHD) requiring immunosuppression MSD and MUD were separated. Incidence outcomes were evaluated using competing risk regression (Fine-Gray method), with death as a competing outcome, while survival outcomes were analyzed using Cox proportional hazards model.
Results: One hundred eighteen B- cell ALL patients were included with a median age at transplant of 43 years (range: 21-69). Donor types included 46 (40.0%) MSD, 45 (38.1%) haploidentical, and 27 (22.9%) MUD. Most were Hispanic (N= 92, 78.0%) and our median follow-up time was 23.6 months. The majority of patients achieved CR1 (N=79, 66.9%) and MRD negativity by flow (N=106, 89.8%), pre-transplant.
The 3-year OS and DFS for the cohort were 82.1% (95% CI 73.8-91.3%) and 66.2% (95% CI 57.2-76.6%), respectively, while the CR1 subgroup was 90.5% (95% CI 83.3-98.3%) and 77.1% (95% CI 67.8-87.7%) respectively.
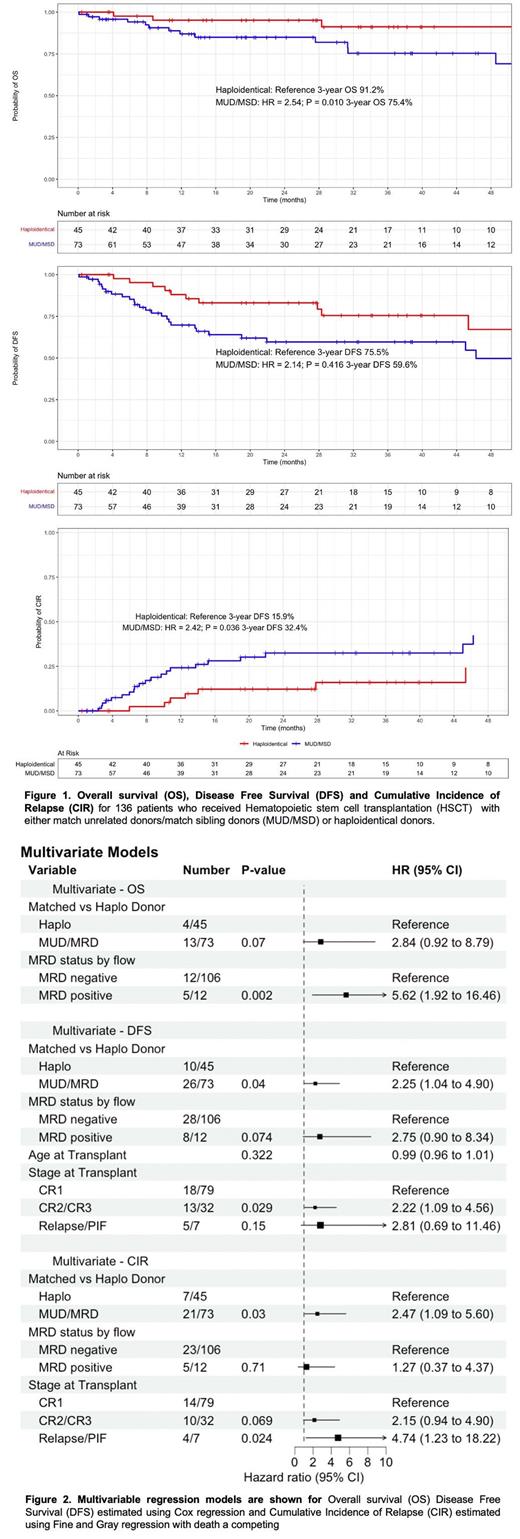
When compared to haploidentical HSCT, patients who received matched donors had significantly worse CIR (HR = 2.42; 95% CI 1.06-5.51; P = 0.036) and DFS (HR = 2.14; 95% CI 1.03-4.44; P = 0.041), along with a non-significant trend towards worse OS (HR = 2.54; 95% CI 0.83-7.80; P=0.10). Additionally, pretransplant minimal residual disease (MRD) positivity demonstrated worse OS (HR = 5.01; 95% CI 1.73-14.5; P = 0.003), DFS (HR = 3.25; 95% CI 1.48-7.16; P = 0.003), and CIR (HR = 2.05; 95% CI 0.78-5.39; P = 0.15).
The 1-year GRFS, 1-year incidence of severe cGVHD, and 100-day incidence of grade 3-4 aGVHD was 52.6% (95% CI 43.5-63.6%), 29.5% (95% CI 20.9-38.6%), and 7.74% (95% CI 3.79-13.5%), respectively. Compared to haploidentical donors, GRFS was worse in the MUD (HR = 2.07; 95% CI 1.08-3.96; P = 0.028) but similar in MSD. This is likely driven by differences in survival and relapse, and there were no differences in the incidence of severe cGVHD or aGVHD between donor types.
Multivariate analysis, which included age, MRD status pretransplant, and stage prior to transplant, demonstrated the improved predictive effect of haploidentical donors. Matched donors exhibited worse DFS (HR = 2.25; 95% CI 1.04-4.90; P = 0.04) and CIR (HR = 2.47; 95% CI 1.09-5.60; P = 0.03), with a trend towards worse OS (HR = 2.84; 95% CI 0.92-8.79; P = 0.07).
Given the heterogeneity in donor-type outcomes, we conducted a subgroup analysis of the 45 haploidentical HSCT patients on the GRFS and DFS composite outcomes. After controlling for patient age, older donor age analyzed as a continuous variable was a significant predictor of worse GRFS (HR = 1.05; 95% CI 1.00-1.11; P = 0.039) but did not affect DFS.
Conclusion: In a predominantly Hispanic population of ALL patients, haploidentical donors demonstrate improved OS and CIR. In those haploidentical patients, younger donor age confers improved GRFS.
Disclosures
No relevant conflicts of interest to declare.